
Cleveland Clinic’s Rohit Chandra Sees Clinical Scribe as First Step in AI Journey
Cleveland Clinic recently selected Ambience Healthcare for AI clinical documentation, with an eye on how these platforms are likely to evolve

Cleveland Clinic recently selected Ambience Healthcare for AI clinical documentation, with an eye on how these platforms are likely to evolve
AHIP (formerly America’s Health Insurance Plans) released a statement yesterday saying that their health plan members “announced a series of commitments to streamline, simplify and reduce prior authorization.” 48 US health plans signed off on the statement. What were AHIP’s 6 commitments? Standardizing Electronic Prior Authorization. Participating health plans will work toward implementing common, transparent submissions…
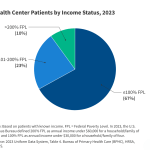
This brief reports on community health center patients, services, experiences, and financing in 2023 and analyzes changes from 2019 (pre-pandemic) through 2023 using data from the Uniform Data System (UDS) and the 2022 Health Center Patient Survey.

Celeste Health Solutions launched on Wednesday. The company works with employers and offers a range of point solutions and provides administrative support. The post How One Company Is Easing Employers’ Administrative Headaches appeared first on MedCity News.
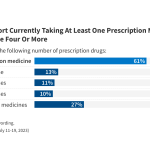
This chart collection draws on recent KFF poll findings to provide an in-depth look at the public’s attitudes toward prescription drugs and their prices. Results include Americans’ opinions on drug affordability, pharmaceutical companies, and various potential measures that could lower prices, including the Inflation Reduction Act.

Three Democratic senators asked the country’s top nonpartisan government watchdog on Tuesday to investigate the costs of a Georgia program that requires some people to work to receive Medicaid coverage. The program, called “Georgia Pathways to Coverage,” is the nation’s only active Medicaid work requirement. Pathways has cost tens of millions in federal and state…

[Sponsored] In this episode, a pharmacy benefit management executive and a pharmacy startup talk about why benefit verification, prior authorizations, and patient affordability still break the workflow and how smart integrations, real-time eligibility, and intuitive design can reduce friction for all involved. The post MedCity Pivot Podcast: Price Transparency is the New North in the…

What happens when payers don’t comply with contract terms? What if a provider overlooks the fine print? Contracts between healthcare providers and payers are supposed to make each party’s responsibilities crystal clear. The reality is often murky. Providers face expensive consequences if they fail to adhere to payer policies – yet they often struggle to…

Acadia Pharmaceuticals did not disclose the buyer of the priority review voucher. The biotech received the voucher last year alongside the regulatory decision that made its drug Daybue the first FDA-approved treatment for the rare disease Rett syndrome. The post Acadia Pharma Sells Voucher for Speedier FDA Drug Review for $150M appeared first on MedCity…

Allara Health’s $26 million Series B raise was led by Index Ventures and included participation from Google Ventures. In total, the company has raised $38.5 million. The post Allara Health Secures $26M to Advance Women’s Hormonal Care appeared first on MedCity News.