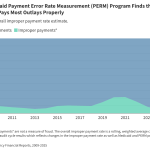
The PERM program measures improper payments in Medicaid through cyclical audits of state Medicaid programs. This brief explains the PERM program and its three component error rates as well as upcoming changes to PERM and possible state impacts.
A Look at the Medicaid Payment Error Rate Measurement (PERM) Program and Upcoming Changes and Impacts